|
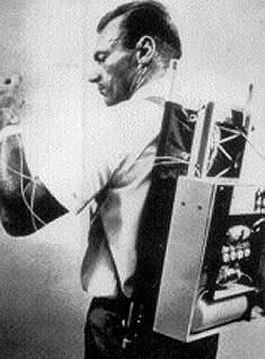
Then: One of the first insulin pumps.

Now: Insulin pump, sensor, receiver.
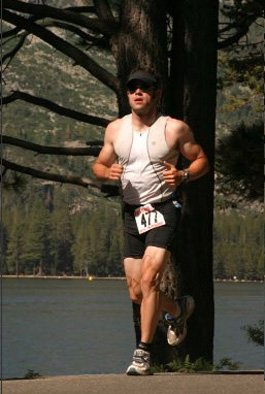
Me finishing a triathlon in Tahoe.
|
May
15, 2006: Sensor Comparison Part 1
The
Artificial Pancreas
What
emotions do you feel after reading the words "artificial
pancreas"? As a person with type 1 diabetes, I have strong
feelings of excitement, relief, and hope. Recently in the
media, the news of continuous glucose sensors has usually
been followed by a statement saying that the artificial pancreas
or closed loop system is right around the corner.
I would
absolutely love to have a device that monitored my BG and
gave insulin automatically, but how soon is "right around
the corner"? Experts are saying 5 to 10 years. However,
I've been promised the same "5 to 10 year" artificial
pancreas timeline since 1990. Has time stopped or have the
estimates been way off? Now that continuous glucose sensors
are available, the idea of an artificial pancreas sounds simple,
right? Unfortunately, an automatic insulin delivery system
is incredibly complicated and technology must overcome some
substantial obstacles. I think it probably won't be available
for at least 10 years..
Since
writing my blog, I have talked to many parents and people
with diabetes who think the artificial pancreas will be available
in the near future (a few short years). Many people have been
disappointed after hearing the realities and obstacles of
an artificial pancreas. Just the other day, one parent told
me that "I was bursting her bubble" after I explained
the obstacles of an artificial pancreas. For this reason,
I think the realities of the artificial pancreas/closed loop
system are very important to discuss. After extensive research,
here's my opinion of what is needed for a true artificial
pancreas.
Definition
of an Artificial Pancreas/Closed Loop System
An artificial pancreas/closed loop system is a mechanical
device that automatically manages and regulates the body's
blood glucose values without input from the user. There are
three components that make up this system: a true real time
blood glucose sensor, faster insulin, and an intelligent software
program. It is crucial that all components of the artificial
pancreas perform with 100% accuracy for 100% of the time.
Component
1: True Real Time Blood Glucose Sensor
This sensor must accurately monitor whole blood glucose values
every minute for 24 hours a day. The Dexcom and other newly
available sensors measure glucose values in the interstitial
fluid. There is a strong correlation between interstitial
fluid and whole blood glucose values. However, whole blood
glucose values are the true indicator of diabetes control
and needed to dose insulin. I've found Dexcom's readings to
be accurate most of the time, but not when my glucose values
are changing rapidly, during exercise for instance (read more
about this lag time: week 1
and week 2 of this blog).
This whole blood glucose sensor will probably be surgically
implanted and replaced regularly to ensure accuracy. Interstitial
sensors are just starting to become available, after years
of development and FDA filings. So I think we are a long way
off from seeing internal whole blood sensors.
Component
2: Faster Insulin
Ultra fast insulins need to be developed for the artificial
pancreas to be effective. The current rapid-acting analog
insulins start working in 5 to 15 minutes, peak in 30 to 90
minutes, and lose effectiveness in 3 to 5 hours. This action
isn't fast enough to normalize rapidly increasing blood glucose
values, especially after meals, for instance. The current
rapid-acting insulin timing can be frustrating and I've run
into serious problems stacking insulin doses (continually
giving insulin to correct a high blood sugar without waiting
for the insulin to run its course) and eventually having a
hypoglycemic reaction. New ultra fast insulins should start
working immediately after delivery and remain active for a
short period of time. These insulins will take time to develop,
test, and receive FDA approval.
Component
3: Software Program/Algorithm
A software program will use glucose information from the sensor
and deliver the correct amount of ultra fast insulin. The
algorithm (complex calculation) for the software program will
need to adapt to the individual's metabolic needs. Each person
with diabetes has unique insulin needs which change according
to activity, stress, and hormone levels. How will the software
program know that I've been increased my activity levels and
require less insulin than I did a week ago? How will the algorithm
account for insulin resistance due to illness? What if the
program malfunctions or delivers too much insulin without
my knowledge? The results could be disastrous if too much
or too little insulin is delivered. Managing type one diabetes
is very dynamic and complex, so the software program must
equally match this dynamic complexity. A few programs are
in development for the artificial pancreas. The data I've
seen showed that one program was able to manage BG levels
while subjects were inactive and fasting, but failed to regulate
BG's during meals. The artificial pancreas' software program
needs to overcome some significant obstacles, which will require
a large amount of time and testing.
Other
Factors
There are three other important issues that the artificial
pancreas must address. First, recent research has revealed
that there is much more to diabetes management than just insulin.
Symlin, for instance, is an important regulatory hormone that
is secreted along with insulin by a fully-functional pancreas.
How will Symlin be incorporated in the artificial pancreas?
Second, if too much insulin is delivered, then there probably
needs to be an emergency glucose delivery system. Lastly,
a person without diabetes' fully-functional pancreas will
start to secrete insulin when that person starts thinking
about eating a meal. Will the artificial pancreas be able
to account for this phenomenon?
Outlook
of the Future
As you can see, diabetes technology must overcome some very
significant obstacles before an artificial pancreas or closed
loop system will be available. If you read or are presented
with the promise of an artificial pancreas, I would ask the
tough questions about the device's three components and other
factors before signing on the dotted line. The idea of an
artificial pancreas gives me hope that the future of my diabetes
won't require fingersticks, insulin dosing, or glucose tablets.
However, hope for the future won't help my diabetes today.
Hope won't help me improve my next HbA1C. Hope won't help
me win my next triathlon this June. Hope certainly won't decrease
my risks for diabetes related complications. In fact, the
future of diabetes is today. The choices I make today will
affect my life and risk for diabetes related complications
in the future.
Don't
worry, not all hope is lost. There are some great tools available
now that make diabetes management much easier than it was
16 years ago. We have rapid-acting insulins, fast glucose
meters that take a pin-sized amount of blood, smart insulin
pumps that calculate and deliver micro-doses of insulin, and
now continuous glucose sensors. Sounds like a great party
to me!
Whether
it's racing triathlons, climbing mountains, traveling to Asia,
or watching TV, I've managed my diabetes using today's tools
and not let the disease slow me down. So I encourage you to
see your diabetes team regularly and pick the best tools for
your diabetes management today.
Regards,
Matt
I do
not work for nor am I compensated by Dexcom in any way. I'm
writing this story because I think continuous glucose technology
is interesting and exciting. Also, I am not a health care
professional and do not give medical advice. I will share
my experiences, but please check with your health care team
before making any changes to your diabetes or health management.
|